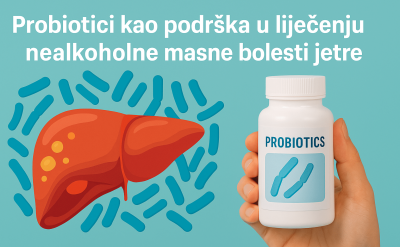
Probiotics as a Natural Ally in Managing Non-Alcoholic Fatty Liver Disease (NAFLD)
Non-alcoholic fatty liver disease (NAFLD) is one of the most common liver conditions in the modern world, affecting people of all ages — including children. It develops in individuals who do not consume alcohol in quantities that could damage the liver and is characterized by excess fat (triglycerides) in liver cells.
Closely linked to obesity, metabolic syndrome, type 2 diabetes, and sedentary lifestyles, NAFLD is considered a manifestation of broader metabolic dysfunction. Conventional treatment focuses on dietary changes, increased physical activity, and weight loss. However, recent scientific attention has shifted toward the gut microbiota’s role in NAFLD development and progression — highlighting probiotics as a promising therapeutic tool.
NAFLD at a Glance: What You Should Know
NAFLD includes a spectrum of liver abnormalities:
• Simple steatosis – fat accumulation without inflammation,
• Non-alcoholic steatohepatitis (NASH) – inflammation, hepatocellular damage, and potential progression to fibrosis, cirrhosis, or liver cancer.
🚨 Major Risk Factors:
• Visceral obesity
• Insulin resistance and type 2 diabetes
• Dyslipidemia
• Hypertension
• Metabolic syndrome
Since NAFLD often develops silently, it’s frequently discovered through elevated liver enzymes or abdominal ultrasound. Early diagnosis is critical to prevent progression.

The Gut-Liver Axis: A Key Connection
The liver and intestines are anatomically and functionally connected via the portal vein, which transports nutrients — and potentially harmful substances like LPS (lipopolysaccharides) — from the gut to the liver.
In healthy individuals, the gut microbiota:
• Maintains homeostasis,
• Supports immunity,
• Regulates metabolism,
• Protects the intestinal barrier.
In NAFLD, however, this balance is disturbed — a condition known as dysbiosis — which can lead to:
• Increased gut permeability (“leaky gut”),
• Systemic inflammation,
• Immune system overactivation,
• Liver stress and disease progression.
🔬 How Probiotics Help in NAFLD: Key Mechanisms
✅ 1. Restoring Gut Microbiota Balance
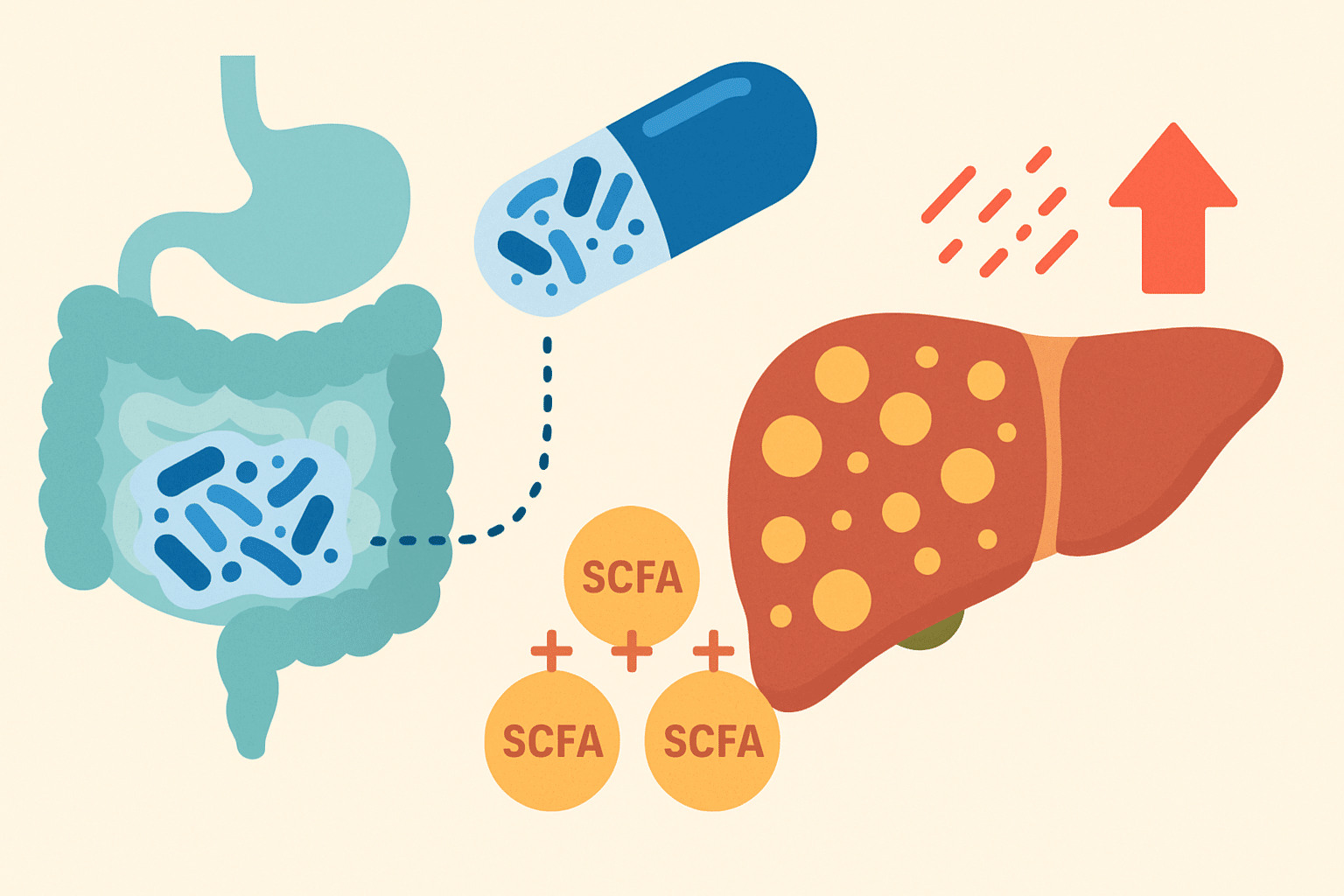
Probiotics help repopulate the gut with beneficial microbes, compete with pathogens, and produce short-chain fatty acids (SCFAs) like acetate, propionate, and butyrate — which:
• Reduce inflammation,
• Improve glucose and lipid metabolism,
• Regenerate intestinal lining.
⸻
✅ 2. Enhancing Intestinal Barrier Function
Probiotics:
• Strengthen tight junction proteins (occludin, claudin, zonulin),
• Boost mucin production,
• Inhibit harmful bacteria.
This reinforces the gut wall, preventing toxic substances from reaching the liver and triggering inflammation.
⸻
✅ 3. Reducing Endotoxemia and Inflammation
LPS from Gram-negative bacteria activates TLR4 pathways, triggering inflammatory cytokines like TNF-α and IL-6.
Probiotics can:
• Break down LPS,
• Downregulate TLR4 expression,
• Increase anti-inflammatory cytokines (e.g., IL-10),
• Suppress NF-κB activity.
This leads to less inflammation and better liver function.
⸻
✅ 4. Regulating Fat and Glucose Metabolism
Probiotics influence:
• Lipogenesis suppression (via SREBP-1c and FAS gene modulation),
• Fatty acid oxidation (via PPAR-α activation),
• Improved insulin sensitivity,
• Lowering triglycerides and LDL cholesterol.
⸻
✅ 5. Antioxidant Support
Oxidative stress accelerates progression to NASH.
Probiotics help by:
• Stimulating antioxidant enzymes (SOD, catalase, glutathione peroxidase),
• Neutralizing free radicals and ROS,
• Reducing lipid peroxidation.
📊 What Does the Research Say?
Recent clinical trials across various age groups and populations show that probiotics can:
• ↓ ALT and AST levels
• ↓ Liver fat (confirmed by ultrasound or MRI)
• ↓ CRP and inflammatory markers
• ↑ Insulin sensitivity (lower HOMA-IR)
• ↓ Body weight and visceral fat
Commonly Studied Probiotic Strains:
• Lactobacillus rhamnosus GG
• Bifidobacterium longum
• Lactobacillus plantarum
• Synbiotics with inulin or FOS
🧪 Synbiotics and Postbiotics: The Next Frontier
🔗 Synbiotics = Probiotics + Prebiotics
They work synergistically to:
• Increase probiotic survival and activity,
• Improve gut ecology,
• Enhance metabolic and anti-inflammatory effects.
Example Combinations:
• L. rhamnosus GG + inulin
• B. lactis + GOS
⚡ Postbiotics: Bioactive Metabolites
Postbiotics are non-living byproducts of probiotic metabolism — like SCFAs, enzymes, peptides, or vitamins — with health benefits even without live bacteria.
They:
• Lower inflammation,
• Reduce oxidative stress,
• Regulate lipid metabolism,
• Strengthen the gut barrier,
• Influence appetite and energy expenditure (e.g., GLP-1, PYY hormones).
📝 Conclusion: Are Probiotics Worth Including in NAFLD Therapy?
Absolutely.
Probiotics — and their advanced forms, synbiotics and postbiotics — offer science-backed benefits that make them valuable allies in NAFLD management. Combined with diet and exercise, they may prevent disease progression and even reverse early damage